An aging population worldwide with the associated prevalence of chronic diseases and late-life disabilities mandates greater emphasis on use of precision medicine in the clinical setting
In 2015, when the Obama Administration announced the Precision Medicine Initiative, a research effort to revolutionize health and disease treatment, it heralded a shift in the traditional “one-size-fits-all” approach to medical treatments. The objective: a tailored approach to patient care that accounts for differences in an individual’s characteristics, environments, and lifestyles, made possible through the use of Big Data, artificial intelligence (AI) and high-performance computing. I maintain that deployment of this critical initiative and a fast track for the innovative technologies that it brings to the market are equally as important in clinical settings as they are in research.
If our reaction to the COVID-19 pandemic has taught us anything, it is that we can harness resources quickly without sacrificing safety in response to a global health threat. Accelerating the approval track for a vaccine could have far-reaching and long-term benefits given the economic, social, and medical impact that its preventative properties provide to at risk populations. The same might be said for widespread use of health data and advanced technologies to identify risk factors, enable faster and more accurate diagnostics, and prescribe treatment under a personalized/precision medicine approach to patient care.
The U.S. Census Bureau’s most recent population projections remind us that by 2030 every Baby Boomer will be age 65 or older. That is 1 in every 5 U.S. citizens, a sobering fact when you consider that within a couple of decades our older population will outnumber children for the first time in our nation’s history. Similar forecasts play out across the worldwide map, demanding action now to forestall a global economic and public health crisis that will have a multi-generational impact with no vaccine to cure. Failure to act now with bold moves to advance public health through faster and more meaningful diagnostics that enable preventative measures could be catastrophic.
These statistics are not new. We’ve known about the impending crisis for some time. COVID-19, however, should be our wakeup call. The pandemic’s level of devastation and medical and economic impact has driven home the point that we cannot rely on protracted years-long studies to find answers. Decision-support technologies and the mass of health data already accumulated can and must be operationalized in clinical practice, and the medical community needs to be educated on effectively integrating technology into their medical practice for a proactive vs. reactive approach to patient care.
Caleb Parry, an 18th century physician once stated, “It is much more important to know what kind of patient has a disease than to know what kind of disease a patient has.” This prescient insight is the basis for Precision Medicine. A focus on the characteristics, the telltale patterns, of a disease state offers predictive value in determining the likelihood of an individual developing a disease, thereby allowing more informed preventative measures and treatments. The value increases with the quality and volume of the data. Software designed with predictive capabilities can ingest and analyze vast amounts of data with a speed and accuracy that no human can, while providing an objective tool for physicians to assess and prescribe individualized therapies that are best suited to their patients’ health and wellness.
There are challenges, of course, in evolving to a machine-learning standard of care, education and cost being at the top of the list. Providers need to be educated on how and when to use it, which should begin in our medical schools with a collaborative effort between tech and medicine. As far as cost, the old adage of “an ounce of prevention is worth a pound of cure” applies. Public and private insurers need to adjust their policies to compensate for use of technology and to allow for potentially higher cost diagnostic and treatment options that offer better long-term outcomes to the patient and significantly reduced healthcare costs over his or her lifetime.
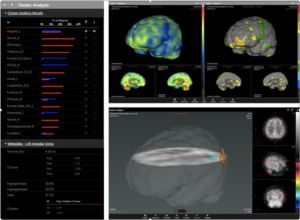
Too tall a task? Can’t be done? I beg to differ. As the CEO of CereHealth Corp., a data analytics technology company that provides Medical Analytics as a Service, I have witnessed firsthand the impact that an objective, accurate diagnosis can have on the economic and social well-being of a patient and their family. Our company, which started as a specialized brain imaging clinic, has taken on some of the most challenging cases involving chronic dysfunction in what is arguably the most complex part of the human anatomy. In doing so we accumulated a mass of structured data that has allowed us to pivot to a focus on applied technologies in a clinical as well as a research setting. The output is nothing short of remarkable. Enhanced insights from CereHealth’s suite of browser-based data analytics tools facilitate dramatically reduced healthcare spending through more objective and personalized diagnostics. By seamlessly integrating digital health data of all types, we enable medical professionals (and researchers) to advise with precision and accuracy the best diagnostic outcome leading to the right treatment for the right patient at the right time in their lives. We arm them with intelligence based on personalized, digitized data used to identify “patients like me”. It is applied science at its best.
While I am frustrated at the pace of progress, I am also encouraged by the great minds working to advance medical technology that I encounter each day in the routine course of our business. A prime example is NanoDX and their patented nanosensor technology platform to detect the presence of biomarker proteins in the blood for quantitative assessment of traumatic brain injury. It is a simple, low cost yet highly accurate system that assesses TBI severity in a 2-minute test, and one example of a pathway forward in effectively integrating data and advanced technologies into routine clinical care. There are many others.
We can and should continue to provide the highest level of patient care here in the U.S. where we have access to the resources to do so. The time is right for rallying those resources and removing barriers so that Precision Medicine becomes the standard for all patients and through it that the promise of a healthier population becomes a model for the rest of the world.
John Kelley is Chairman and CEO of CereHealth Corp. CereHealth has two primary data analytics platforms: CereMetrixAI, a leader in quantitative imaging analysis for central nervous system disorders, and illumeAI, which utilizes graph technology to enable high-performance computing and multivariable analysis and creates correlations among patient and other datasets.